When medical experts call something “inoperable,” most patients feel their hope collapsing. Yet, medical history has proven again and again that innovation can redefine what’s possible. This was the case for Karla Flores, a 19-year-old young woman who became the first patient in the world to undergo what is now called Third Nostril Surgery. This groundbreaking approach gave her a chance to survive a tumor that was considered life-threatening and nearly impossible to remove by conventional means.
What makes Karla’s story especially powerful is not just the science behind it—it’s the human courage, the painstaking teamwork, and the willingness to challenge decades of tradition in neurosurgery. Her case isn’t just one more medical success story; it is a beacon of hope for patients who are told, “there is nothing more we can do.”
Table of Contents
The Origins of the “Third Nostril” Technique
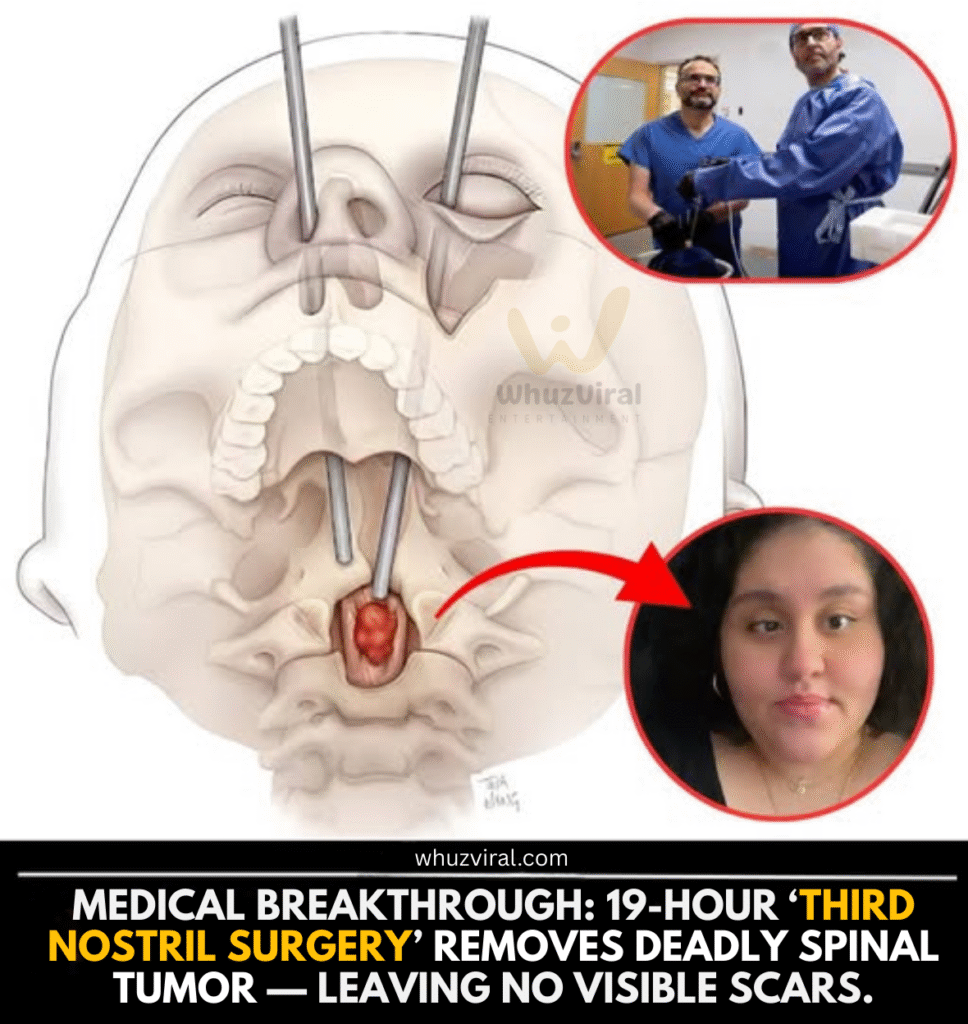
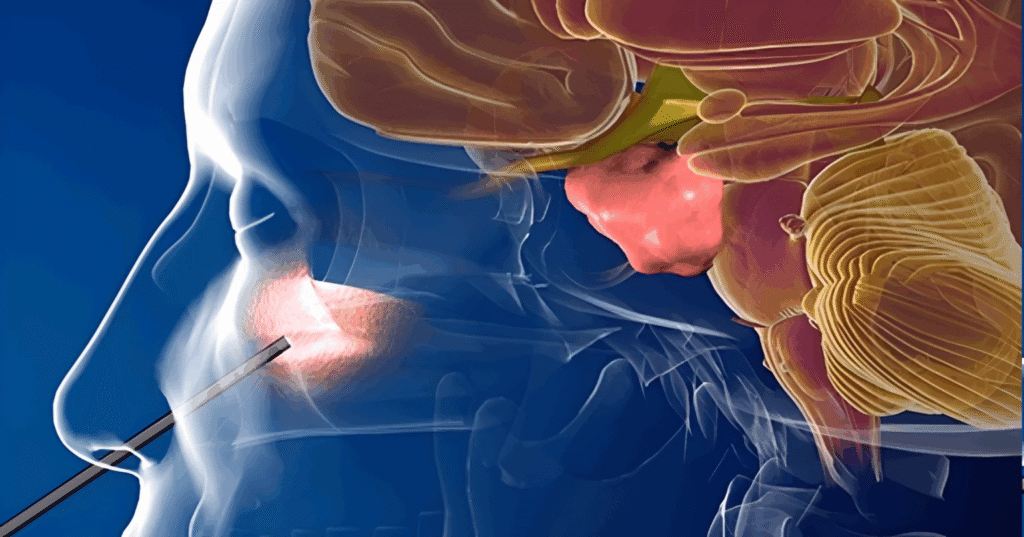
The name Third Nostril Surgery might sound unusual, but the logic behind it is straightforward: surgeons create a new, hidden pathway into some of the most inaccessible parts of the body. The procedure was pioneered by Dr. Mohamed A. M. Labib, a neurosurgeon at the University of Maryland Medical Center. Instead of entering through the skull, neck, or nasal cavity—each of which carries significant risks—Dr. Labib conceptualized a corridor through the patient’s eye socket. This corridor became the so-called “third nostril.”
Traditional approaches to the craniocervical junction (the meeting point of the brain and spine) require navigating through dense bone, critical blood vessels, and clusters of fragile nerves. Every millimeter of error risks paralysis, loss of speech, or death. By rethinking anatomy and embracing cutting-edge reconstruction techniques, Dr. Labib and his team avoided many of these dangers entirely.
The vision for this technique didn’t come overnight. It was the product of years of anatomical study, cadaver practice, and interdepartmental collaboration. Surgeons had to not only remove the tumor but also restore the face and orbital bones in a way that preserved both function and appearance.
Karla’s Personal Journey
Karla’s story begins like many others: with symptoms that didn’t seem too alarming at first. At just 18, she began experiencing double vision. For many, this could point to something as harmless as eye strain or astigmatism. But as her vision issues worsened, doctors ordered imaging scans—and the results were devastating. Karla had not one, but two chordomas, a rare type of bone tumor that typically grows near the skull base and spine.
Her doctors knew the tumors would be exceptionally difficult to remove. The first tumor, near her brainstem, was approached with a traditional craniotomy. The second, lodged at the craniocervical junction, was deemed far more dangerous. Standard surgery came with life-threatening odds.
Faced with this reality, Karla could have given up. Instead, she placed her trust in a surgeon who was willing to attempt the impossible.
Inside the 19-Hour Operation
Every step of Karla’s surgery was carefully choreographed. The procedure stretched across 19 hours, involving a multidisciplinary team of neurosurgeons, plastic surgeons, anesthesiologists, and nurses.
The team began by carefully entering through Karla’s lower eyelid and cheekbone. Unlike traditional surgeries that leave visible scars, this method relied on precise internal incisions. Surgeons removed sections of her orbital floor and part of her cheekbone. They gently shifted her eyeball aside—not damaging it, but creating a corridor into the depths of her skull.
Through this corridor, surgeons navigated directly to the tumor. Working millimeter by millimeter, they carefully removed it, ensuring no damage to the surrounding brainstem or spinal cord. Once the tumor was out, the focus turned to reconstruction.
To rebuild her face, the surgical team used titanium plates to stabilize her orbital area. Bone grafts taken from her hip replaced the sections of bone removed from her cheek. The end result was astonishing: Karla’s facial structure looked natural, her eye was preserved, and her scar was virtually invisible.
Watch: “Third Nostril” Surgery in Action
This video shows how surgeons at the University of Maryland Medical Center used an eye-socket approach—known as Third Nostril Surgery—to remove a dangerous spinal tumor. Credit: University of Maryland Medical Center / YouTube
Why the “Third Nostril” Approach Matters
This surgery represents far more than a single patient’s triumph. It signals a potential shift in how neurosurgeons worldwide might approach tumors that were once deemed inoperable.
The advantages are clear:
- Scar-free recovery: Unlike traditional craniotomies or facial incisions, Third Nostril Surgery leaves no visible scars.
- Avoiding critical structures: Surgeons can bypass the jugular vein, eustachian tube, and key cranial nerves.
- Direct access: The “straight line” corridor through the eye socket provides more precise navigation to the tumor site.
- Reduced risk: By minimizing disruption of surrounding tissue, the risk of complications decreases.
For patients and their families, these benefits are life-changing. A diagnosis that once meant living with a deadly tumor can now come with a renewed chance at life.
Karla Today: A Future Reclaimed
Karla is now cancer-free. Her recovery hasn’t been without challenges—she has some lingering nerve damage that affects the movement of her left eye—but overall, her prognosis is excellent. More importantly, she is alive, thriving, and planning her future.
Despite facing an overwhelming medical bill of nearly $600,000, Karla’s spirit remains unbroken. She is determined to pursue her dream of becoming a professional manicurist. Her resilience is as inspiring as the surgery that saved her.
Her case is now being hailed as a turning point in modern neurosurgery, one that could redefine what patients around the world might expect when facing tumors once thought impossible to remove.
Voices Behind the Breakthrough
After surviving the marathon 19-hour surgery, Karla described her relief in a way that resonates deeply:
“When they told me I had a tumor in a place too dangerous to operate, I thought my life was already over. But Dr. Labib gave me hope. Waking up and realizing I was alive—and that I had no scars—felt like a miracle. I know I still have healing to do, but I finally see a future again.”
Her words reflect both the fear of her diagnosis and the gratitude she feels for her surgical team.
Karla’s mother shared the emotional burden of watching her daughter go through something so rare and dangerous:
“No parent is ready to hear that their child has a tumor doctors say can’t be removed. We felt powerless. But this surgery gave us our daughter back. The courage of the doctors and Karla’s strength through all of this have been nothing short of inspiring.”
Families often endure as much emotional pain as the patient themselves, and her mother’s words highlight the sense of renewed hope.
Dr. Mohamed Labib, who pioneered the Third Nostril Surgery, expressed humility in the face of such groundbreaking achievement:
“This surgery was not about me—it was about Karla. It was about finding a way to save her life when the conventional options posed risks that were simply too great. What we did was create a new pathway, but her strength and trust carried us all through the long hours in the operating room.”
He also acknowledged the collaborative effort of the team:
“A surgery like this is never the work of one person. It takes neurosurgeons, plastic surgeons, anesthesiologists, nurses, and every member of the team giving their all. This is why medicine advances—because we dare to ask, ‘What if there’s another way?’”
Karla’s case has already inspired patients worldwide facing similar diagnoses. One commenter on a hospital forum wrote:
“Reading about Karla made me cry. I was told last year my tumor is too deep to remove. Now I feel hope again. Maybe this new technique could save me too.”

A Look at the Science Behind Chordomas
Chordomas are rare, slow-growing tumors that originate from remnants of the embryonic notochord. While they grow slowly, their location—often near the brainstem or spinal cord—makes them extremely dangerous. They account for only about 1% of brain tumors, but their impact is disproportionately severe.
Traditional treatment options include surgery and radiation therapy. However, complete removal is often difficult because of the tumor’s proximity to critical nerves and blood vessels. Even when removed, chordomas can recur. This is why Karla’s case is so extraordinary: the surgeons not only removed the tumor but did so in a way that minimized long-term damage and scarring.
The Human Side of Medical Innovation
Behind every medical breakthrough is a human story of perseverance—not just from the patient, but also from the surgeons and medical staff. For Dr. Labib, developing the Third Nostril Surgery required years of study, courage to attempt something new, and trust in his team.
Karla, meanwhile, had to make a leap of faith. Agreeing to an experimental surgery is not easy, especially when the alternative might seem safer, even if less effective. Her bravery, combined with the dedication of her medical team, is what turned this once unthinkable idea into reality.
What This Means for the Future of Neurosurgery

Medical experts believe that Third Nostril Surgery could open doors for treating a wide range of conditions, not just chordomas. Tumors at the skull base, upper spinal cord, and even certain vascular malformations might one day be approached through this technique.
If widely adopted, this could mean:
- Shorter recovery times for patients.
- Less need for invasive procedures.
- Better cosmetic outcomes.
- A higher success rate for removing complex tumors.
It’s still early, and the technique is currently limited to highly specialized medical centers. But as more surgeons are trained and more cases are documented, the potential for global adoption grows stronger.
Frequently Asked Questions (FAQs)
What is Third Nostril Surgery?
Third Nostril Surgery is a revolutionary neurosurgical technique that allows surgeons to access deep-seated brain and spinal tumors through the eye socket, avoiding large external incisions and visible scars.
Who developed this technique?
The procedure was pioneered by Dr. Mohamed A. M. Labib and his team at the University of Maryland Medical Center.
Is Third Nostril Surgery safe?
While all surgeries carry risks, this approach reduces many of the dangers associated with traditional methods. By avoiding critical brain and spinal structures, the likelihood of serious complications decreases.
Will patients have scars after surgery?
No. Because the entry point is through the eye socket and internal facial structures, patients do not have visible external scars after the operation.
Is this surgery available worldwide?
Currently, it is limited to advanced academic medical centers. However, as the technique gains recognition, it may spread to hospitals worldwide.
How long is the recovery?
Recovery times vary depending on the patient and the complexity of the tumor. However, because this method avoids large incisions, patients generally heal faster than with traditional surgery.
What types of tumors can be treated this way?
The approach is especially promising for chordomas and other tumors located at the skull base or craniocervical junction. Future studies may expand its use to other tumor types.
Final Thoughts
Karla’s story is more than a medical milestone—it’s a testament to human resilience and the power of innovation. The fact that a tumor once considered inoperable was removed without leaving a scar shows how far medicine has come.
The phrase “Third Nostril Surgery” may sound unusual today, but in the future, it could become as familiar as “open-heart surgery” or “laparoscopy.” And when it does, we will remember that it all began with a 19-year-old girl who refused to give up and a surgeon who dared to imagine a new way forward.
The ICC’s Charges Against Rodrigo Duterte
Introduction: When Domestic Power Meets International Justice On a humid September morning in 2025, news…
A Father’s Burden: Turning in His Own Son, Tyler Robinson, in Charlie Kirk Case
Nine days ago, lives changed forever on the campus of Utah Valley University. A public…
Groundbreaking “Third Nostril Surgery” Saves 19-Year-Old from Deadly Spinal Tumor
When medical experts call something “inoperable,” most patients feel their hope collapsing. Yet, medical history…
🚨 Ghost Flood Control Project in Bulacan: Marcos Orders Blacklist and Legal Action Against Contractor
Video: President Ferdinand “Bongbong” Marcos Jr. inspects the alleged ₱55-million “ghost” reinforced concrete river wall…
China Drone That Flies and Swims: 7 Stunning Facts About the Shape-Shifting SeaDuck
In a coastal testing facility near Shandong, China, a team of engineers has achieved what…
Nearly 4,000 Undocumented Filipinos Face Deportation from the US: A Wake-Up Call for OFWs
🧭 Introduction: Why This Matters to Every OFW As an OFW currently teaching English in…